CATEGORIES
RECENT POSTS
LifeBio Memory Group Classes are Just Pure Fun November 15, 2024
LifeBio Memory Group Classes are just plain FUN November 15, 2024
3 Memory Care Programming Tips November 15, 2024
TAGS
- reminiscence therapy activities
- reminiscence and brain fitness
- reminiscence group
- life story group
- life story classes
- reminiscence class
- brain fitness class
- amazing stories
- autobiography classes
- classes for seniors
- intergenerational class
- older adult curriculum
- older adult ministry
- reminiscence classes
- writing an autobiography
- memory care programming
- activities for memory care
- social history for people with dementia
- create a legacy
- lifestories
- seniorcare
- seniorliving
- Life Story Program
- cognitive screening
- activities for dementia
- alzheimers
- cognitive testing
- Dr. Richard Morgan
- spiritual autobiography
- reminiscence therapy
- life story
- lifebio
- alzheimer's
- Alzheimer's
- Dementia
- Depression
- Journals
- Legacy
- MyHello Line
- Person-centered care
- Positive Brain Health
- Recall
- Remember
- Reminiscense Therapy
- RT
- senses
- What's Your Story?
- Record life stories
- combat loneliness
- personalized medicine
- occupational therapy and reminiscence therapy
- life stories for hospice patients
- life stories for palliative care
- partnership
- 2022
- post-covid
- workforcecrisis
- Loneliness Intervention
- sdoh
- lifestory
- agetech
- LifeBio research
- memorial day
- A Veterans Story
- world war ii
- Social Connectedness
- farfromalone
- interview mother
- mother's day
- Longevity, Health, & Innovation
- lifebiobrain
- MyHello
- healthtech
- conscious aging
- growing older
- vietnam veterans life stories
- vietnam
- national vietnam war veterans day
- deuce and a half
- army
- vietnam war
- veterans day
- vietnamtruckdriver
- vietnam truck driver
- veterans administration
- vietnam veterans and health care
- true love
- narrative spirituality and aging
- life story work
- friendship model
- build relationships
- love your neighbor
- keep going
- seniors
- loneliness
- Overcome
- Motivation
- Teepa Snow
- startuphealth
- StartUp Health Magazine
- LOVE STORY
- LifeBio
- LifeBio Memory
- LifeBio ALZ
- Family Stories
- Thanksgiving
- National Family Stories Month
- Reminiscing
- Keep the conversation going
- Dewey K
- Clarendale of Mokena
- Life Story
- Veteran
- National Alzheimer's Awareness Month
- National Family Caregivers Month
- LifeBioALZ
- nostalgia
- alzheimers disease
- digital therapeutic
- memory care
- dementia care
- nonpharma solutions
- healthy aging
- life stories
- legacy
- healthy aging month
- using reminiscence in health care
- using reminiscence in hospice
- volunteer programs for long-term care
- sister
- sisters
- friends
- biography
- autobiography
- story
- stories
- real
- biographical stories
- farm life
- raising butterflies
- teacher
- teaching
- true
- write
- writing
- career
- nurse
- medical
- job
- work
- Loneliness
- Isolation
- Solitude
- Aging
- Planting seeds
- Growing Family
- Apple Tree
- innovator's pitch challenge
- life science nation
- mary furlong & associates
- What's Next Longevity Venture Summit
- Sense of Time
- Not too late
- what will you do with your time
- Save family stories
- Online biography
- Sharing family stories
- covid-19
- pandemic
- isolation
- hope
- telephone interviews
- lifebio online options
- Guideposts article
- Benjamin Rose Institute on Aging
- living legacy
- family history
- telling your story
- Biography
- For people living with Alzheimer's or dementia
- Record memories
- quality care for memory loss
- love
- life
- meaning
- Fun at Work Day
- Coffee Cup
- How to fill your cup
- I choose happiness
- Storytelling
- LifeBio Reminiscence Method
- Innovator's Pitch Challenge
- IPC
- 39th Annual JP Morgan Healthcare Week
- Positivity
- Gratitude
- Blessings
- New Years resolutions
- Goals
- Happy New Year
- 2020
- New Year 2021
- Remembering 2020
- Hindsight is 2020
- To auld lang syne
- to days gone by
- Artificial Intelligence
- Northwestern University Master of Science in Artificial Intelligence 2020
- LifeBio Cares
- The Gables
- Messages of Hope
- LifeBio Book Covers
- New LifeBio Book Cover Designs
- Mourning the loss
- Christmas story
- personal story
- Life stories in health care
- reminiscence and health care
- Psychiatrist Dr. Robert Butler
- Life as story
- storytelling as self-discovery
- reminiscence
- reminscence with memory challenges
- overcome loneliness
- LifeBio Memory Journal
- Narrative as social connector
- Storying Later LIfe G. Kenyon
- The Narrative Complexity of Ordinary Life by W. Randall
- Celebrate holidays while socially distant
- Celebrate christmas while quarantined
- creative ways to celebrate holidays
- Playing Games over videoconference
- Tell life story
- Christmas gift ideas for elderly
- Connect through Music
- reminisce
- Social engagement
- brain health
- social brain
- thanksgiving
- give thanks
- gratitude
- Family Caregivers
- Caregivers
- Care for Caregivers
- Military
- Veterans Life Story
- history
- WWII
- Small Business Innovation Research grant
- SBIR grant
- National Institute of Aging
- Research Roundup
- Reminiscence
- remember
- memories
- life stories in senior living
- life biography
- Success Stories
- Caring for caregivers
- Family
- extended family
- immediate family
- family memories
- certification
- Women Owned
- National Women's Enterprise Business Certification
- Women's Business Enterprise National Council
- WBENC
- interesting
- social isolation
- meaningful interaction
- social distancing
- positive thinking
- positivity
- reminiscing
- Memories
- Dogs
- Pets
- Music therapy
- Reminiscence therapy
- Life story
- Olympics
- getting started
- sharing life stories
- Family stories
- Remembering
- Life stories
- cycling
- cycle
- bicycle
- bike
- ride
- MyHelloLine
- Changing Lives
- Intervention
- Telephone calls
- Group calls
- Person to Person Calls
- Check in calls
- Amy's Story
- Bev's Story
- Social Calls for seniors
- Senior Citizen daily calls
- Communications with seniors
- Reminiscing questions
- Connected living
- Intergenerational
- Student Intern calls
- Summer memories
- phrases
- constellations
- dogs
- reminiscing memories
- remembering
- good questions to ask
- my lasting legacy
- reminiscing questions
- Fourth of July
- July 4th
- 4th of July
- Cookout
- Parade
- Fireworks
- Celebrate
- Celebration
- Get-togethers
- Family gatherings
- Family reunion
- Patriotic
- Picnic
- Veterans
- Bonfire
- Firecracker
- Beach
- Independence Day
- Traditions
- Autobiography
- Reminiscing memories
- Family history
- Personal Historian
- My lasting legacy
- Holiday memories
- Emotional Wellness
- Redemption Stories
- Resiliency
- Online templates
- senior living communities
- emotional well-being
- Memory care
- Self-care
- Stress reduction
- Inner strength
- Self-awareness
- Positive thinking
- Resilience
- Brain science
- Meditation
- Self-affirmation
- Mindset
- Stress management
- Connectivity
- Avoid Social Isolation
- Decrease Depression
- Spanish calls
- English calls
- Encore
- Gateway Community Action
- Foster Grandparents
- Gateway Foster Grandparents
- Father's Day
- Making Decisions
- Telling Your Story
- Sharing Accomplishments
- Giving Advice
- Avoid Head Injuries
- Brain Health
- Cognitive Decline
- Diet
- Exercise
- Healthy Alcohol Consumption
- Journal
- Mental Stimulation
- Reminiscence Therapy
- Sleep
- Social Contacts
- Wellness Checks
- Writing
- Decoration Day
- Honor Fallen
- How Will You Celebrate
- Memorial Day
- Memorial Day History
- Not Forgotten
- Poppies
- Remember Their Stories
- Ultimate Sacrifice
- What is Memorial Day
- Adversity
- Advice
- Facing Hardships
- History
- Sharing Your Story
- Unique Story
- Free Conversation Group
- Phone Call
- Zoom Call
- Communication Tips
- How to Act
- How to Ask Questions
- How to Respond
- How to Speak
- Positive
- Preparation
- Reminisce
- What Not to Say
- What to Say
- Beth Sanders
- Covid-19
- Logan Plaster
- YouTube interview
- gifts
- Laurel's story
- Mom
- Mother's Day
- Ask yourself
- Connect
- Covid-19 response
- Creativity
- Healthy body
- Healthy mind
- Move
- Outside
- Quarantine
- Self-isolation
- Six Questions
- Social distancing
- acknowledge
- coronavirus
- distance
- eye contact
- isolated
- wave
- Care packages
- Creative Ideas
- Letters
- Memberships
- Music
- Photos
- Share Memories
- Show and Tell
- Videoconference
- What's Your Story? cards
- How to
- Tutorial
- Typing your story
- Using LifeBio website
- Audio Recording
- Document a life story
- Family tree
- Save photos
- Tell a Life Story
- Write a Life Story
- Your Love Story
- Personalized Story
- Sharing your story
- Storymaker
- Storyteller
- Storytelling quotes
- dementia
- phone communication
- telephone questions
- Connecting
- Conversation Starters
- Coronavirus Response
- Covid-19 Response
- Epidemic
- Meaningful Interaction
- Social Distancing
- Social Isolation
- Biographical Stories
- Capture Your Story
- Mental Health
- Social Interation
- Writing Prompts
- Friendship
- REMINISCE
- TELL YOUR LIFE STORY
- UNIQUE VALENTINE'S DAY GIFT
- VALENTINE'S DAY
- butcher shop
- errands
- Illinois
- My Life Story
- Writing Your Story
- Biography Examples
- How do I write my biography
- How to write a biography
- Where to wite my biography
- Free biography
- How to write my story
- Write my story
- Music Therapy
- Music Therapy Services
- senior health care services
- Person Centered Care Services
- hungary
- veteran story
- russion gulag
- Home
- GI
- letter
- Lonely
- tips for overcoming loneliness
- Story
- Life Stories
- Naidex
- how to write a biography
- how to write an autobiography
- personal biographer
- tell your story
- writing a biography
- activities
- grandchildren
- grandparents
- sharing your story
- tell your life story
- active aging
- Healthcare
- health care
- senior living
- skilled nursing
- volunteering
- wellness
- activities for senior living
- Activity
- Elderly
- Seniors
- activities for the elderly
- activity directors
- person centered care
- wellness for seniors
- Christmas
- Kesges
- happy
- memory
- cow
- dog
- cat
- pet
- favorite
- elvis
- presley
- famous
- Autobiography template
- sample autobiography
- writing an autobiography made simple
- about me
- children's hospital
- genealogy
- journaling
- kids
- narrative exposure therapy
- teens
- terminal illness
- ethical will
- heartfelt letter
- if I die letter
- letter to my loved ones
- priceless gift
- the ultimate gift
- Alzheimer's disease
- memory book
- memory loss
- interviewing a veteran
- questions to ask a veteran
- veteran's life story
- veterans day activities
- veterans history project
- writing a veterans life story
- reminiscence is therapeutic
- therapeutic reminiscence
- last wwi veterans dies
- wwii veterans life stories
- dementia activities
- dementia therapy
- memory care activities
- reminiscence in memory care
- memory books to capture this is my life
- this is my life in retirement communities
- how do I tell my grandma's life story?
- biography template
- write my biography
- writing my biography
- how do i interview my mother my father my grandma my grandpa
- 5 tips for writing an autobiography
- if i die
- ifidie
- recording christmas memories
- writing christmas letters
- writing christmas stories
- fdr speech about pearl harbor
- pearl harbor attack remembered
- pearl harbor speech
- 10xelerator
- Fisher College of Business
- The Ohio State University
- wakeup startup
- veterans story
- best holiday gifts for grandparents
- top holiday gifts for grandma 2011
- top holiday gifts for grandpa 2011
- what should I get my grandparents for christmas?
- best gifts for financial advisors to give to clients
- financial advisor client gifts
- gifts under $20 from financial planners
- holiday gifts for financial advisors
- 10 years after September 11
- 2001
- memories of September 11
- mother's memory of Sept. 11
- people in ohio remember september 11
- true colors lyrics
- creative assisted living
- creative retirement
- retiring in an rv
- veterans biography questions
- veterans day program ideas
- veterans story book
- veterans storybook
- wwii veteran life stories
- pat summitt basketball coach
- lifebio iphone
- lifebio mobile
- intergenerational programming
- intergenerational programming in nursing homes
- intergenerational programming in senior living
- intergenerational programs in churches
- life stories in retirement communities
- technology for retirement communities
- technology solutions for senior living
- journaling for people with memory loss
- journaling for PTSD
- journaling health benefits
- journaling to help with depression
- memory books for alzheimer's
- aarp video
- amazing videos
- generation y video
- lost generation
- rethinking reminiscence
- ageism
- baby boomers aging
- dr. bill thomas
- memorial day for veterans
- memorial day program ideas
- veterans stories
- adult day programming for retirement communities
- cognitive impairment in retirement communities
- memory care curriculum
- lifebio.com
- online autobiography template
- alzheimer's and boomers
- alzheimer's disease facts
- standup gardens
- great gift ideas for mother's day 2011
- life story journal
- memory books for mother's day
- memory gift box
- memory journal
- she calls me raymond
- how to create a lasting legacy
- ice cream memories
- life story writing
- storycorps mobile booths
- storycorps oral history
- studs terkel
- how to write life stories of my grandparents
- interviewing dad
- interviewing grandma
- interviewing grandpa
- interviewing mom
- geriatric psychiatry and life stories
- intergenerational communications
- advantages of storytelling
- my life story
- storytelling around the campfire
- storytelling for grandparents
- storytelling for parents
- storytelling to our children
- storytelling to our grandchildren
- unique 70th birthday gifts
- unique 80th birthday gifts
- unique birthday gifts for seniors
- earthquake and tsunami relief
- volunteers capturing life stories
- volunteers doing oral history interviews
- statistics on aging
- activities for grandparents and grandchildren
- grandma's life stories
- grandpa's life stories
- memories of grandparents
- tell us a story grandma
- tell us a story grandpa
- activities for grandparents
- baby books and grandparents
- recording memories for grandchildren
- creating a lasting legacy
- ethical will template
- legacy letter
- writing my life story
- frank buckles dies
- wwi veteran death
- brain fitness and dementia
- dementia care tools
- reminiscence therapy and dementia
- reminiscence therapy tools
- the notebook and dementia care
- capture life stories
- capture your own life story
- example of life stories
- rehab therapy and reminiscence therapy
- rehabilitation therapy and reminiscence therapy
- speech therapy and reminiscence therapy
- person-centered care
- eden alternative
- eden at home
- living with dementia
- memories of elders
- activities for adult day care centers
- adult day care activities
- ideas for activities in adult day programs
- journaling with dementia patients
- capturing memories
- how to talk with older people
- loneliness in boomers and seniors
- writing my memoir
- writing your life story
- intergenerational projects for kids
- intergenerational projects for teenagers
- intergenerational projects for teens
- intergenerational projects for youth
- autobiography class for libraries
- autobiography writing group
- autobiography writing group in libraries
- daptive technology for assisted living
- adaptive technology for skilled nursing
- computers for assisted living
- computers for nursing homes
- technology for nursing homes
- activities for alzheimer's
- alzheimer's activities
- life stories in memory care
- conversation starter games
- family gathering games
- family reunion games
- games for a reunion
- reunion games
- shower games
- memories lost or forgotten
- record memories for people with alzheimer's disease
- record memories for people with dementia
- autobiography class for all ages
- autobiography class for older adults
- autobiography class for seniors
- reminiscence therapy for alzheimer's patients
- writing down memories for alzheimer's patients
- record your life stories
- record your life story
- bible studies for boomers
- bible studies for seniors
- bible study for boomers
- bible study for seniors
- intergenerational Bible study
- interview your grandparents
- snow day activities
- snow day activity
- what can teenagers do when school is closed
- overcoming hate with love
- problem solving
- world peace
- personal historian in ohio
- life story curriculum for memory care
- reminiscence curriculum for alzheimer's disease
- activities for early-stage alzheimer's
- life stories for early-stage Alzheimer's disease
- reminiscence for early-stage alzheimer's disease
- life review and reminiscence for people with alzheimer's
- memory books for people with alzheimer's
- reminiscence therapy for people with alzheimer's
- storytelling for people with dementia
- life stories work and social work
- social work and life stories
- social workers and life stories
- using reminiscence in social work
- life review and social work
- life stories and geriatric care management
- listening is an act of love
- tips for writing life stories
- activities with grandchildren
- how to make bread
- tips for baking bread
- create a memory book
- family life stories
- life story book
- world war ii stories
- life stories of parents
- oral history interview
- recording parents
- writing dad's life story
- writing mom's life story
- life stories in long term care
- life stories in nursing homes
- video recording in senior living
- writing autobiographies in senior living
- best gift ideas
- christmas gifts
- gifts for dad
- gifts for grandma
- gifts for grandpa
- gifts for mom
- gifts for parents
- hanukkah gifts
- wellness director
- wellness programming
- wellness trends
- ethical will kit
- how to write an ethical will
- legacy letter kit
- writing an ethical will
- life bio journal
- writing my autobiography
- teaching children how to work
- tips for teaching hard work
- volunteer experiences for kids
- what is an ethical will
- autobiography template
- activities in retirement communities
- new programs for retirement communities
- intergenerational programs in libraries
- libraries and family history projects
- oral history projects in libraries
- norman rockwell memories
- sweet memories
- best client gifts
- best gifts for financial planners to give to clients
- top 3 client gifts
- reminiscence and psychiatry
- reminiscence and psychology
- life story journals
- life story tools
- memory training program
- life stories for senior living
- new activities for nursing homes
- new activities for skilled nursing
- oral history tips
- veteran's story
- activity program in long term care
- assisted living
- activities for nursing homes
- autobiography classes for seniors
- computer programs for seniors
- autobiography for hospice patients
- biography for hospice patients
- reminiscence therapy for hospice patients
- activities for seniors
- ICAA successful programs for older adults
- wellness programs for older adults
- financial advisor gifts
- financial planner gifts
- gift ideas for clients
- conducting an oral history
- oral history recording
- reminiscence therapy for recreation therapy
- oral history questions
- tools for reminiscence therapy
- aarp
- activity programs for seniors
- great depression
- great recession
- video recording a biography
- video recording kit
- 3 tips for activity directors
- activity connection
- activity ideas
- aging and wellness
- brain fitness
- retirement
- social engagement
- narrative care
- narrative medicine
- innovative activity program
- lifelong learning
- 4 tips for activity directors
- long term care activities
- reminiscence therapy tool
- wellness program
- brain fitness and memory care
- memory care program
- reminiscence and memory loss
- memory care programs
- retirement community memory care
- brain fitness and reminiscence
- reminisce magazine
- retirement communities
- biography book
- personal history
- dementia programming
- memory book for alzheimer's
- reminiscence and life review
- autobiography how to
- dr. barry baines
- life story gift
- treasures of the heart
- group biography class
- uided autobiography class
- life review classes
- senior center classes
- guided autobiography
- home health and reminiscence
- reminiscence and hospice
- older americans month
- online autobiography
- write autobiography
- writing a memoir
- writing memoir
- motivational interviewing
- caregiver communication
- gerontology
- tips for writing an autobiography
- journal of memories
- unique graduation gift
- autobiography of mom
- family celebrations
- family history and genealogy
- family reunion fun
- association of personal historians
- oral history
- oral history genealogy
- fun with grandkids
- grandchildren activities
- memory journals
- caregivers
- caregiving
- family reunions
- icaa
- masterpiece living
- keepsake autobiographies
- keepsake journal
- memory books
- senior activities for activity directors
- senior living programs
- wellness programs for seniors
- building community
- friendly visit
- friendly visit ideas
- friendly visiting program
- senior service innovations
- CCRC
- disorientation
- geriatric depression
- retirement community
- brain fitness programming
- retirement communities and brain fitness
- retirement communities and wellness
- autobiography classroom project
- emotional intelligence
- social and emotional education
- products for older adults
- asa
- boomer summit
- chicago
- 7 tips for writing your autobiography
- genealogy journal
- telling my life story
- tipe for writing autobiography
- how to autobiography
- Boy Scouts of America
- phone recording interviews
- Interview grandma
- interview grandpa
- capture memories
- travel journal
- positive aging
- how to create a memory book
- how to record life stories
- intergenerational oral history
- recollections
- how to interview dad
- interview mom
- interview parents
- cheap autobiography
- easy autobiography
- aging
- biography writer
- writing autobiography
- phone recording
- write your life story
- aarp lifestyles
- writing biography
- autobiography writer
- personal historians
- youth group ideas
- creative memories
- life stories in churches
- unique bible study
- digital scrapbooking
- write a book
- national day of listening
- storycorps
- eid
- Hanukkah
- memorable gifts
- unique gifts
- neurology
- interviewing grandparents
- interviewing parents
- retirement living
- audio recording
- recording memories
- autobiography gift
- gift of autobiography
- active aging week 2009
- international counceil on active aging
- end of life
- living will
- biography gift
- how to write an autobiography video
- interview dad
- unique gift of autobiography
- interview father
- interview grandparents
- grandparents memories
- aahsa
- life care services
- celebration of life
- funerals
- life celebration
- memory book for dementia
- scrapbooking
- write biography
- Baby boomer marketing
- David Weigelt
- ImmersionActive
- marketing to baby boomers
- social media
- autobiography book
- reunion
- Lifebio certified community
- twibes
- $1
- 000 contest
- tell your life story contest
- tell your story contest
- interviewing father
- interviewing mother
- life sto
- unique father's day gift
- unique mother's day gift
- baby boomers
- social capital
- marketing events
- outreach events
- speaker
- easter
- family gatherings
- father's day
- gift of memories
- family stories
- generations
- DIY autobiography
- do-it-yourself autobiography
- genealogists
- 50+ ministry
- boomer ministry
- building small groups
- older adult ministries
- senior ministry
- press room
We Have a Need for Speed: Innovations in Agetech
Posted By: Beth Sanders | Posted On: 20 April, 2022
The Numbers
Right now there are approximately 54 million people in the US over the age of 65. By 2040, that number is projected to rise to 80.8 million, and then to 94.7 million in 2060. 5.8 million Americans were living with Alzheimer’s disease in 2020. That number will nearly triple unless something changes by 2060.
In the meantime, the caregiver shortage keeps getting worse. A report from the Global Coalition on Aging (GCOA) and Home Instead Senior Care outlines how a national shortage of 151,000 caregivers will exist by 2030, increasing to a 355,000 caregiver shortage by 2040.
What are we going to do?
Although baby boomers hold over half the nation’s wealth and the aging population represents a clear and growing market, investment in new technologies serving the aging market is relatively new. Even the terms "agetech" or "longevity tech" are relatively novel. Part of the hesitancy relates to doubt that older people will utilize digital tools. But the amount of money people over the age of 65 spend on technology during the pandemic is helping put some of that skepticism to rest. According to AARP, older adults spent on average $1,144 on new technology, up from $394 in 2019.
The investment world is starting to take notice. In 2020, funding to U.S. startups focused on creating products/services for this aging population grew to $1.1B after a fairly steady four-year average around $390M. The primary focus of these investments relate to healthcare, particularly B2B businesses that provide care services, but as ‘aging in place’ grows momentum as a movement and with the care industry struggling to find staffing, there is a necessary shift happening. Money is starting to move towards getting people healthier sooner and keeping them healthier for longer, with an emphasis on supporting better Social Determinants of Health (SDoH) like social connectedness, access to food/transportation/good housing and Personal Determinants of Health (PDoH) like resilience, optimism, and purpose. Science is just now starting to understand how much these PDoH impact both the quality and the length of life, and the money is slowly starting to follow. Mental health is certainly tied to physical health.
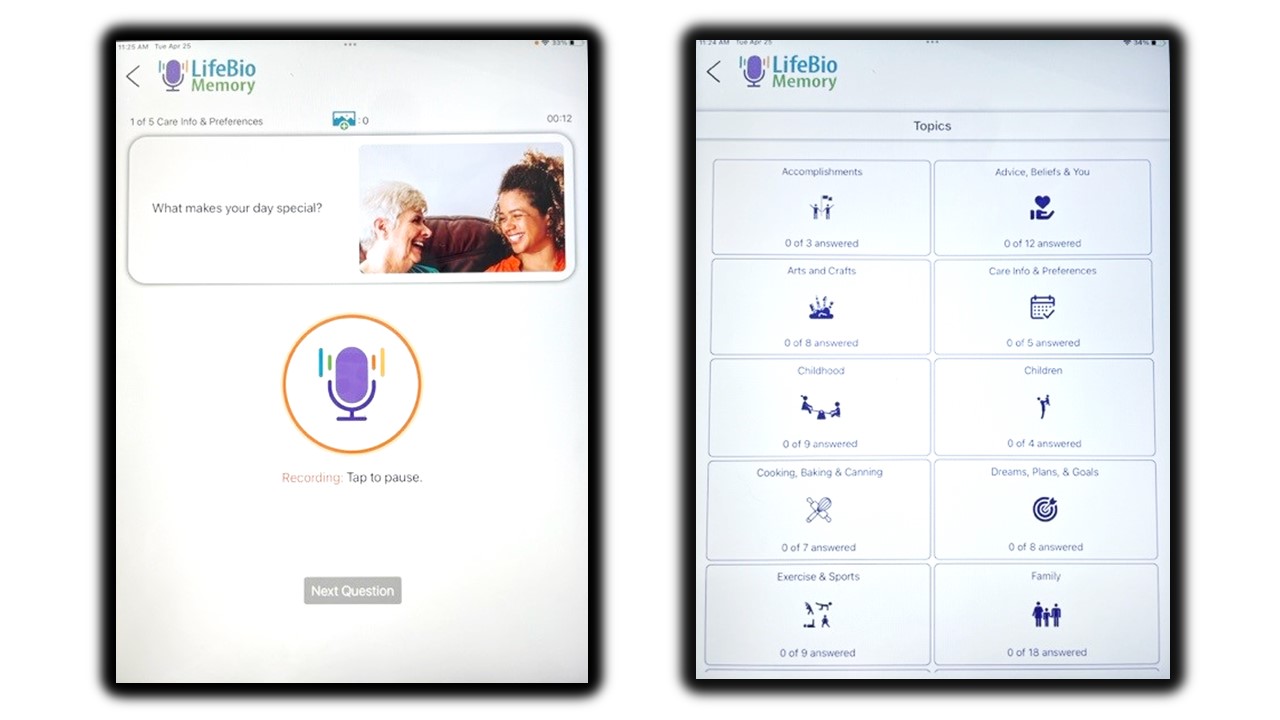
SDoH technology could look like an app that helps seniors access transportation to health care appointments, or one that makes grocery deliveries simple. Or it could be an online fitness program that takes into account joint health, arthritis or other common health concerns in an older population (Spiro100 for example). There are digital tools showing success at addressing issues like loneliness, isolation, and the need to create meaning (our app, LifeBio Memory, is one of them or MyHello, our tech-powered loneliness intervention). Even screening for dementia is something that needs more attention which means a new app being born as we speak, LifeBio Brain, is working with clinicians on a prototype and early user trial.
What are we waiting for?
Perhaps the question isn’t “What are we going to do?” but rather “What are we waiting for?” We actually know what needs to happen. We need people to get and stay healthy or as Dr. Rick Moody coins the need for awareness as one ages---"conscious aging." We need tools that reduce the burden of care on families as more people age at home, and for the overloaded staff for those in senior living. We need to prioritize connection and community as significant drivers of health. We need to broaden our sense of what is possible in an aging population.
The pandemic spurred a seachange in how older adults are using technology. This provides us with a chance to explore digital ways to serve this population. There’s momentum growing, not only with investors but with the government to back innovation in this arena. Just this past month, bipartisan legislation was introduced in Congress to expand Medicare coverage to include Prescription Digital Therapeutics (PDTs) (Access to Prescription Digital Therapeutics Act of 2022). If this bill is passed, the ramifications for elder care would be huge. PDTs have proven effective at treating depression, addiction, anxiety and other mental health issues. They are part of a holistic healthy aging plan, “social prescriptions,” in which doctors refer patients to community resources that support overall wellbeing and don’t just prescribe medications.
The point is, all options should be on the table right now. There is a huge need to rethink what aging can and should look like…and a huge opportunity to meet this challenge with creative solutions that address the whole person—mind, body, and soul. We see the future and we are working to keep up with the immense needs now and in years to come.